The virus lurks in the dorsal root ganglion like a terrorist waiting. Blindsided and forgotten like chickenpox, when it surfaces, the shingles’ rash can look like an alien reptile has left its imprint on your skin and is sometimes referred to as “the devil’s grip.” The varicella-zoster virus has shadowed the human race for thousands of years causing chickenpox and later in life shingles. Although researchers are investigating the phenomenon of the herpes virus’s unique ability to replicate itself, as of yet, no known cure exists to oust it from the body, where it dwells in the ganglia and, along with other unwanted guests, in the liver. The best solution, like dealing with a difficult mother-in-law, is to coexist.
Shingles has increased and is four times as common now as it was sixty years ago. “It’s increased across all age groups,” says Dr. Barbara Yawn, Chief Scientific Officer at COPD Foundation.
Doctors still don’t know the reason for the increase. “We’ve done studies, and we just don’t know,” Dr. Yawn says. “The increase is not due to greater rates of immuno-suppression in the population, not due to lack of boostering, not due to introduction of the chickenpox or varicella vaccine, not due to more doctor’s visits, and not due to access to anti-viral meds.”
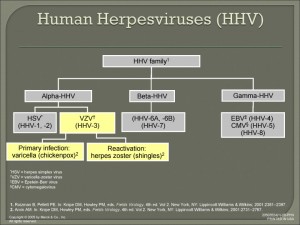
The viruses herpes-zoster (VZV) and herpes simplex (HSV), the one that causes cold sores, are neurotropic alpha viruses that live in clusters of nerve cells near the spine called the dorsal root ganglion; the ganglia is the connection between the nerves coming out of the spinal cord and the peripheral nerves.
There’s some indication VZV thrives on stress. “I suppose some of it could be due to more widespread stress,” Dr. Yawn says. “We know that there’s increased risk of shingles in people who have had adverse life events.”
In fact, Dr. Yawn’s study Risk Factors for Herpes Zoster revealed that female sex, race/ethnicity, family history, and co-morbidities such as asthma, diabetes, and COPD, are risk factors for HZ.
“The herpes zoster and the herpes simplex is a fascinating family of viruses,” says Dr. Yawn. “They all act in a similar way that they stay dormant for years and don’t cause any symptoms but then can reactivate.” The viruses hide in the nerve tissues, replicating, surviving, waiting, until the right time, when the immune system is weakened, to spring into action.
Viruses can also sleep in the liver. Dr. Jeffrey Cohen, Chief of the Medical Virology Section in the Laboratory of Clinical Infectious Diseases at the National Institute of Allergy and Infectious Dieseases, in Bethesda, Md. says, “The latent VZV along the spine should be the same as VZV that’s sometimes detected in the liver as far as we know. Hepatitis viruses (A,B,C) infect the liver, and other viruses less commonly infect the liver. The vertebra of the spine can also be infected by bacteria including tuberculosis, and some fungi can occasionally infect the vertebra and cause abscesses.”
Another member of the family is the cytomegalovirus (CMV), a common virus most people don’t know they have, because it rarely causes symptoms. Once CMV is in the body, like all herpes, it takes cover in the ganglia. According to the CDC, “Among every 100 adults in the United States, 50–80 are infected with CMV by the time they are 40 years old.” Yet another relative is the Epstein-Barr virus, that causes infectious mononucleosis or mono as it’s known. Dr. Cohen says that, “CMV can occasionally infect the spine,” too.
There is not a definitive association of EBV and COVID-19 or zoster and COVID-19. While there are anecdotes of persons with both infections at or near the same time, this does not prove there is a direct association between them. The possibility of COVID’s link to herpes is under the microscope. New studies prove that Long Covid variants can live in the body for up to a year and impact the overall immune system. Additional reports with similar features are needed for a true association, experts say.
It’s essential to keep VZV from reactivating. “The only way is the shingles’ vaccine,” says Dr. Yawn. “But the vaccine hasn’t been studied in people younger than fifty and so does not have FDA approval. Shingles and complications like postherpetic neuralgia are less common in people under fifty and many people would need to be vaccinated to prevent one case or one complication.”
How can we supercharge our immune system to fight off the enemy? “There’s no magic potion,” says Dr. Yawn. “Some people need to use immuno-suppressive medications for cancer, to prevent rejection of transplanted organs, or to treat some chronic diseases like moderate to severe rheumatoid arthritis. But for people without these needs, avoiding stress, treating depression, having a healthy, well-balanced diet, activity, and maintaining a normal weight can help.”
Alternative options can strengthen the immune system, too. Dr. Mary Claire H. Wise, Integrative Family Physician, recommends milk thistle supplements to support the liver and the metabolic detox pathways in the liver. “When you’re not holding on to toxins, your immune system is able to function better,” says Dr. Wise. “For herpes viruses, what I have found works best is L-lysine three grams daily, St. John’s Wart 450mg twice a day, and echinacea one gram three times a day to prevent a recurrence.”
Kiki Flynn, the popular YouTube Wellness Guru and Lifestyle Coach, recommends neem supplements, because neem is anti-viral, anti-fungal, and anti-bacterial. Neem mitigates parasites, eczema, and viruses like shingles. In India, neem trees grow up to fifty feet high, a symbol of health, wealth, and community well-being. But, advises Kiki, “Check with your doctor and do not take if pregnant or nursing. Take according to label and do not exceed two weeks.”
To detox the liver, Kiki recommends her castor oil deep cleanse pack at Kiki Says.
